Breast augmentation, also known as augmentation mammoplasty, is a surgical procedure designed to enhance the size, shape, or fullness of a woman’s breasts. It’s one of the most common cosmetic surgeries in the United States, supported by decades of research, technological advances, and evolving safety protocols.
For many women, breast augmentation is deeply personal: restoring volume lost after pregnancy or weight loss, improving symmetry, enhancing self-confidence, or simply achieving a silhouette they feel better aligns with their identity.
However, it’s not a decision to take lightly. Success depends on understanding anatomy, implant options, risks, recovery, emotional impacts, cost, and selecting the right surgeon. This article dives into all that helping you make an informed, empowered choice.
1. Why Women Choose Breast Augmentation
Before discussing the how, it’s important to understand the why. What motivates someone to undergo breast augmentation? These are the most common reasons in the U.S.:
-
Restoring volume lost due to pregnancy, breastfeeding, major weight loss.
-
Improving symmetry, especially when one breast is noticeably smaller or shaped differently.
-
Changing shape or projection — wanting fuller cleavage, a different silhouette under clothes.
-
Boosting self-esteem and body confidence, especially when self-image feels affected.
-
Reconstruction — after mastectomy, injury, or congenital abnormalities.
These are valid, powerful reasons. But the best outcomes tend to come when the decision is based on realistic expectations and personal desires, not just outside pressure or trends.
2. Overview: What Happens During Breast Augmentation
Here’s a step-by-step look at what breast augmentation involves:
2.1 The Consultation
-
Assessment of your health history: any past surgeries, pregnancies, breastfeeding, weight fluctuations, underlying medical conditions.
-
Examination of chest anatomy: breast size/shape, skin quality, chest wall shape, existing asymmetry.
-
Discussion of goals: desired size (cup size vs actual cc’s of implants), feel (soft vs more firm), profile, implant placement.
-
Review of implant types, shapes, textures, incision options, and any additional procedures you might need (e.g. lift if there’s sagging).
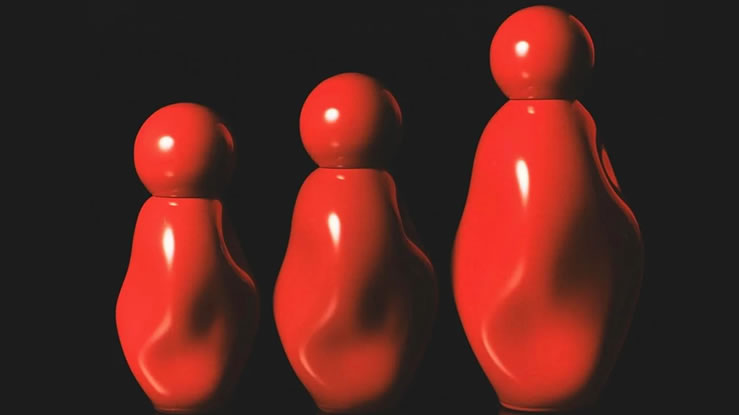
2.2 Types of Implants
The U.S. Food & Drug Administration (FDA) currently approves two main types of breast implants:
-
Saline-Filled Implants: A silicone outer shell filled with sterile saltwater (saline). FDA-approved for augmentation in women 18 or older. U.S. Food and Drug Administration+1
-
Silicone Gel-Filled Implants: A silicone shell filled with silicone gel. FDA-approved for augmentation in women 22 or older. Many prefer it because it tends to feel more like natural breast tissue. U.S. Food and Drug Administration+1
Other implant variations include:
-
Gummy Bear / Form-Stable Implants: Silicone implants with firmer gel that holds shape even if shell is broken; more stable structure but require larger incision. American Society of Plastic Surgeons
-
Round Implants: Softer, fuller at the top, no danger if they rotate. American Society of Plastic Surgeons
-
Textured vs Smooth Surface Shells: Textured surfaces were once popular to reduce risk of certain issues, but FDA and health bodies are stricter now due to correlations between textured implants and Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL). U.S. Food and Drug Administration+1
2.3 Placement, Incisions, and Profile
-
Implant Placement:
-
Subglandular (above chest muscle, below breast tissue)
-
Submuscular (partially or fully under chest muscle)
-
-
Incision Sites:
-
Inframammary (under the fold of the breast)
-
Periareolar (around the nipple)
-
Transaxillary (under the arm)
-
Transumbilical (rare; “belly button” incision – less common).
-
-
Profile / Projection: How far the implant projects from the chest wall: low, moderate, high, extra high. Profile selection affects how dramatic vs natural your results will look.
2.4 The Surgery Itself
-
Performed under general anesthesia typically.
-
Surgery time: usually ~1-2 hours depending on complexity, placement, and whether additional procedures (like lift) are included.
-
After surgery: wounds closed, dressings applied, support bras used.
3. Safety, FDA Rules, and Latest Advances
Knowing the risks and what’s new helps you make safer decisions.
3.1 FDA Safety Requirements & Labeling
-
In October 2021, the FDA updated safety requirements and risk communication. Manufacturers must provide clearer labeling, risk information, and data from long-term studies. U.S. Food and Drug Administration+1
-
Approved implants must have updated labeling regarding possible risks, certification, performance data (Summary of Safety and Effectiveness Data: SSED). U.S. Food and Drug Administration+1
3.2 Known Risks & Complications
According to the FDA, complications can include but are not limited to: U.S. Food and Drug Administration+1
-
Capsular contracture, scar tissue around implant hardens.
-
Implant rupture or deflation (especially silicone ruptures may be “silent”).
-
Pain, changes in nipple or breast sensation (temporary or permanent).
-
Asymmetry or unsatisfactory aesthetic outcome.
-
Infection.
-
Wrinkling / rippling (visible tattoos or skin see-through).
-
Rare but serious: BIA-ALCL (a type of lymphoma), rare cases of other cancers or squamous cell carcinoma around implant capsules. U.S. Food and Drug Administration+1
3.3 Recent Implant Approvals & Innovations
-
Mentor MemoryGel Enhance Implants (silicone gel) recently approved for U.S. for reconstruction with very large volumes/widths (930 cc to 1445 cc), of importance for patients who require larger implants (body frame, reconstruction after mastectomy). JNJ.com
-
Increased focus on device tracking, post-approval studies, long-term performance, especially for “silent rupture,” using MRI or ultrasound monitoring. U.S. Food and Drug Administration+2U.S. Food and Drug Administration+2
3.4 Longevity of Implants and Replacement
-
No implant is lifetime-guaranteed. The risk of needing revision increases with time. Replacement or removal may be required due to complications or aesthetic changes. U.S. Food and Drug Administration+1
-
Recent research (e.g. ultrasound elastography) shows implants tend to become stiffer over time (e.g., 8 years + depending on usage) which may lead to rupture risk. arXiv
4. The Emotional, Psychological, & Physical Impact
It’s not just about the body; breast augmentation carries emotional weight.
4.1 Positive Impacts
-
Increase in self-confidence and positive body image.
-
Feeling more “proportionate” or aligned with personal aesthetic ideals.
-
Improved post-pregnancy or post-weight loss body satisfaction.
4.2 Possible Emotional Challenges
-
Body image expectations vs reality: sometimes final results don’t match vision.
-
Recovery phase discomfort, swelling, expectation management.
-
Post-surgery anxiety: how the body looks, feels, changes over time.
-
Influence of societal pressures, social media, partner expectations.
4.3 Relationship With Aging, Weight Changes, Pregnancy
-
Skin elasticity decreases with age; older individuals may need lifts or revisions sooner.
-
Significant weight changes after surgery can stretch skin and affect implant position.
-
Pregnancy and breastfeeding might alter breast shape, even with implants.
5. Recovery: What to Expect, Care, and Timeline
Detailed look at what life looks like in recovery and how to get the best outcome.
5.1 Immediate Post-Surgery (Week 1)
-
Expect swelling, bruising, discomfort, tightness in chest. Pain managed with medication.
-
Rest and limited upper body movement. Avoid lifting, pushing, pulling.
-
Wear support or surgical bras per surgeon’s instructions.
5.2 Weeks 2-4
-
Gradual return to light normal activity. Avoid strenuous exercise.
-
Follow up visits to check healing, remove stitches (if any), inspect for complications.
5.3 Months 1-3
-
Swelling reduces; implants “settle” into final position. Final shape begins showing.
-
Light massage / scar care as recommended to reduce visibility of incisions.
5.4 Long Term (3-12 months and beyond)
-
Full healing, sensation recovery can take several months.
-
Ongoing check-ups. Monitor for signs of complications.
-
Supportive bras part of long-term wear to help maintain shape.
6. Cost: What Breast Augmentation Costs in the U.S. in 2025
Cost is a big factor below are current ranges, what affects pricing, and budget considerations.
6.1 Typical Cost Ranges
-
Average breast augmentation with implants cost in the U.S.: $7,000 to $15,000+, depending on location, surgeon’s expertise, implant type, combined procedures (e.g. augmentation + lift). Examples from real patients: quotes in the $8,000-$16,000 range. Reddit+1
-
More extensive surgeries or premium surgeons in high-cost regions (NYC, LA, etc.) can push costs higher.
6.2 What Drives the Cost
-
Surgeon’s fee (board certification, experience, reputation).
-
Hospital or surgical facility fees.
-
Anesthesia.
-
Implant cost (silicone implants often more expensive than saline).
-
Additional procedures (lift, fat grafting, symmetrization).
-
Post-operative care, garments, follow-ups.
6.3 Financing and Insurance
-
Cosmetic breast augmentation is usually not covered by insurance unless it is reconstructive (post-mastectomy, congenital deformity, etc.).
-
Many surgeons offer financing plans or work with medical loan companies.
7. How to Choose a Surgeon and Plan Safely
Choosing who does the surgery matters a lot for safety, satisfaction, and minimizing regret.
7.1 Credentials and Board Certification
-
Look for a board certified plastic surgeon (American Board of Plastic Surgery – ABPS).
-
Check membership in professional societies (American Society of Plastic Surgeons – ASPS).
7.2 Before & After Photos & Patient Reviews
-
Ask to see photos of people with similar body types and desired outcomes.
-
Read reviews and, if possible, talk to previous patients.
7.3 Detailed Discussion of Implant Options
-
Discuss implant type (silicone vs saline), shape (round vs anatomical), profile, size (cc’s).
-
Discuss incision location and placement.
-
Talk about textured vs smooth shells, given current safety info.
7.4 Facility Safety & Follow-Up Care
-
Ensure the surgical facility is accredited.
-
Ask about aftercare, revision policy, emergency protocols.
-
Discuss long-term monitoring: imaging (MRI or ultrasound) to check for ruptures, inspections.
8. Alternatives & Non-Surgical Options
If you’re unsure about implants or want less invasive methods, there are alternatives, though each has trade-offs.
-
Fat Transfer: Taking fat from another part of your body and injecting into breasts. More natural look; limited increase.
-
Non-Surgical/Filler Options: PRP (platelet rich plasma), injectable fillers, Morpheus8, Sculptra etc these can help shape, lift a little, improve texture, but usually cannot achieve large size increases. Example: “Cleavage Clinic” in NYC offering non-surgical “natural boob jobs” for $2,900-$7,000. New York Post
9. Recent Trends (2025) in Breast Augmentation
What’s changing, what’s being approved, what people are asking for:
-
Larger silicone implants approved (Mentor MemoryGel Enhance: up to 1445 cc for reconstructive use). JNJ.com
-
More women wanting natural-looking results moderate size increases with emphasis on proportion rather than dramatic volume.
-
Increased concern and information sharing about textured implants and risks of BIA-ALCL.
-
Non-surgical or minimally invasive augmentation gaining traction in demand.
-
Better implant tracking, more transparent risk communication and updated labeling required by FDA (2021 onwards). U.S. Food and Drug Administration+2U.S. Food and Drug Administration+2
10. What Questions Should You Ask Yourself & Your Surgeon
To help you decide, here are guiding questions:
-
What is my ideal size and shape, and why do I want that? (Vision + realistic goals)
-
Am I okay with possible trade-offs (scarring, changes in sensation, revision surgeries)?
-
Do I have medical issues (autoimmune, connective tissue disorder, prior chest surgery) that might complicate things?
-
How much downtime can I realistically take? What’s my recovery plan?
-
What is the total cost (surgeon + facility + implants + aftercare + potential future revisions)?
-
What safety features does the implant have (shell texture, shape, post-approval studies, monitoring)?
11. Case Studies / Real Stories (Short Examples)
-
A patient choosing between silicone vs saline implants, describing differences in feel, cost, and follow-ups.
-
A patient who underwent fat transfer instead of implants, with pros & cons.
-
A reconstruction patient needing large size implant (using Mentor MemoryGel Enhance) after mastectomy, her decision process.
(These help readers relate personally.)
12. Pros & Cons Summary
| Pros | Cons |
|---|---|
| Enhances self-esteem, body confidence | Surgery risks (infection, complications) |
| Ability to choose size, shape, and projection | Possible need for future surgery or revisions |
| Better symmetry and restoring lost volume | Cost can be high; not always covered by insurance |
| Advances in implant types, more natural feel | Possible complications: capsular contracture, rupture, changes in sensation |
| Many years of safety data and regulatory oversight | Long-term maintenance, possible replacements needed |
Breast augmentation is a deeply personal, powerful procedure. For many U.S. women, it offers a path to restore balance, confidence, or simply feel more aligned with their body’s identity. But the best outcomes come when every angle is considered: physical health, emotional readiness, surgeon credentials, safety, realistic expectations, and long-term commitment.
If you’re considering breast augmentation in 2025, use this guide:
-
Know your goals and reasons.
-
Research implant types and safety.
-
Choose your surgeon wisely.
-
Understand recovery & cost completely.
-
Be ready for long-term follow-ups and possible future changes.
Ultimately, the most important “augmentation” is what happens inside how you feel, how you love yourself, and how you move forward with confidence.
Related Articles