Diastematomyelia Type 1 is a rare congenital spinal disorder that affects the alignment and development of the spinal cord. It belongs to a broader group of neural tube defects and is characterized by a longitudinal split or duplication of the spinal cord, usually caused by a bony or fibrous septum. While this condition is uncommon, it is important to understand the proper diagnostic steps, treatment methods, and long-term care approaches — especially for Type 1, which is the more complex and symptomatic form of the condition.
This article explains how Diastematomyelia Type 1 is treated, including medical and surgical interventions, the role of imaging and diagnosis, and the long-term prognosis for individuals diagnosed with this condition.
Read Also >>>What is firatlift type 1?
Understanding Diastematomyelia Type 1
Diastematomyelia, often referred to as split cord malformation (SCM), occurs when the spinal cord is divided into two hemicords. The condition is usually classified into two types:
-
Type 1 (Complex SCM): Involves two dural sacs and a rigid septum (usually bony or cartilaginous) that divides the spinal cord. This form is often associated with other spinal anomalies such as scoliosis, tethered cord, or lipomas.
-
Type 2 (Simple SCM): Involves a single dural sac with a fibrous or non-rigid septum dividing the cord.
Type 1 is the more severe variant and often causes neurological symptoms early in life. It typically requires more aggressive treatment, including surgical correction, to prevent long-term damage.
Causes and Risk Factors
Diastematomyelia is a congenital condition, meaning it develops during fetal growth. The exact cause is not entirely understood, but it is believed to result from abnormal development of the notochord and neural tube in early embryogenesis.
Risk factors include:
-
Genetic mutations or chromosomal abnormalities
-
Maternal diabetes or poor nutrition during pregnancy
-
Environmental exposures during early gestation
Because it is typically diagnosed in childhood or early adolescence, early detection and intervention are crucial.
Symptoms of Diastematomyelia Type 1
The symptoms can vary depending on the extent of the spinal cord split and the structures involved. Common signs include:
-
Back pain
-
Lower limb weakness or asymmetry
-
Gait abnormalities or clumsiness
-
Scoliosis (curved spine)
-
Incontinence or bladder dysfunction
-
Cutaneous markers on the back (such as a dimple, hairy patch, or skin discoloration)
Type 1 is more likely to present with neurological deficits due to tethering or compression caused by the bony septum.
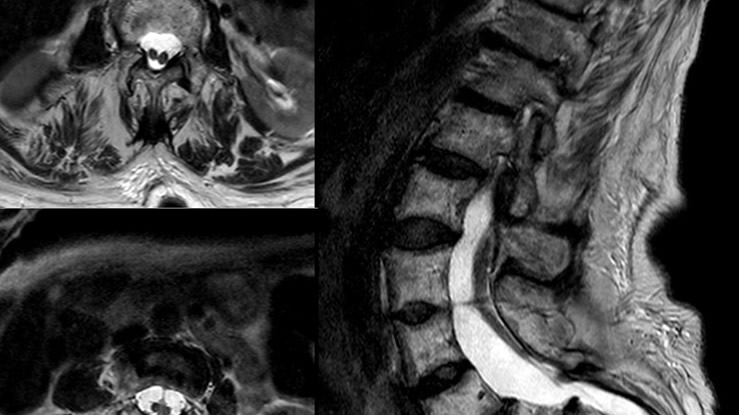
Diagnosing Diastematomyelia Type 1
Accurate diagnosis requires a combination of clinical evaluation and imaging studies. Most cases are identified in early childhood due to signs such as scoliosis or motor weakness.
Key diagnostic tools include:
-
MRI (Magnetic Resonance Imaging): The gold standard for diagnosis, showing the split cord, septum, and associated anomalies.
-
CT Scan (Computed Tomography): Used to identify bony structures, such as the osseous spur or rigid septum.
-
X-rays: May reveal spinal deformities like scoliosis or vertebral anomalies.
-
Ultrasound: Sometimes used in neonates or young infants before ossification is complete.
Early diagnosis is essential to minimize complications, particularly those associated with progressive neurological deterioration.
Treatment of Diastematomyelia Type 1
Treatment depends on the severity of symptoms and the presence of neurological impairment. For Type 1, surgery is the standard course of treatment, especially when there is evidence of spinal cord tethering or compression.
1. Surgical Intervention
Surgical correction is recommended in most cases of Diastematomyelia Type 1, especially when symptomatic. The goal is to:
-
Remove the bony or fibrous septum
-
Release the tethered spinal cord
-
Untether associated abnormalities (such as lipomas or dermoid cysts)
-
Restore normal cerebrospinal fluid flow
Common procedures include:
-
Laminectomy or Laminoplasty: Removal or reshaping of part of the vertebra to access the spinal cord.
-
Excision of the Septum: Surgical removal of the bone or cartilage dividing the spinal cord.
-
Dural Reconstruction: If the spinal cord is within two dural sacs, surgeons may repair or unify them for better support.
Postoperative monitoring is crucial to detect complications like cerebrospinal fluid leaks, infection, or worsening of neurological symptoms.
2. Neurological Monitoring
During surgery, intraoperative neuromonitoring (IONM) is typically used to ensure that the spinal cord and nerves are not damaged. This allows the surgical team to adjust the procedure in real-time to protect function.
3. Management of Associated Conditions
Diastematomyelia Type 1 is often found in conjunction with:
-
Tethered Cord Syndrome
-
Spina Bifida Occulta
-
Chiari Malformation
-
Hydromyelia
Each of these conditions may require additional surgical or non-surgical management. Comprehensive treatment planning often involves a multidisciplinary team including neurosurgeons, orthopedic surgeons, and neurologists.
Non-Surgical Management
In some rare, asymptomatic cases — especially if the septum is fibrous and not causing compression — close observation may be considered.
Non-surgical care includes:
-
Regular neurological assessments
-
Physical therapy for muscle strength and coordination
-
Bladder training or management for urinary issues
-
Scoliosis monitoring and orthopedic care
However, for Type 1 cases, non-surgical management is usually temporary or supportive, as surgery is often ultimately necessary to prevent progression.
Recovery and Rehabilitation
Recovery after surgery for Diastematomyelia Type 1 typically involves:
-
Hospital stay of 3–7 days
-
Physical therapy to regain strength, mobility, and coordination
-
Follow-up imaging to monitor surgical success and spinal cord function
-
Neurological exams to track improvement or any residual symptoms
Children often recover well with early intervention, while delayed treatment can result in permanent deficits. Full recovery timelines can vary but often take several months.
Long-Term Outlook and Prognosis
When treated early, most patients with Diastematomyelia Type 1 experience significant improvement in symptoms and quality of life. Key factors influencing prognosis include:
-
Age at diagnosis
-
Severity of neurological symptoms
-
Presence of additional spinal anomalies
-
Effectiveness of surgical correction
In cases where surgery is delayed or complications arise, the patient may face ongoing neurological issues, such as weakness, incontinence, or chronic pain.
Potential Complications
Even with surgery, some risks remain:
-
Re-tethering of the spinal cord
-
Spinal instability after bone removal
-
CSF leaks or infection
-
Residual or worsening symptoms if nerves are already damaged
These risks highlight the importance of experienced surgical teams and regular post-operative monitoring.
Parental and Patient Support
For children diagnosed with Diastematomyelia Type 1, early parental education is essential. Support groups, physical therapy, and regular follow-ups contribute to long-term success. Adolescents may require counseling or additional support during puberty, especially if scoliosis or bladder dysfunction impacts daily life.
Research and Future Treatment Advances
Although Diastematomyelia is rare, research into neural tube defects and spinal anomalies is ongoing. Innovations in neurosurgery, such as robotic-assisted procedures, improved imaging techniques, and regenerative therapies, may enhance treatment outcomes in the future.
Scientists are also exploring the genetic and molecular basis of spinal cord malformations to potentially prevent or treat these defects during early development.
Diastematomyelia Type 1 is a rare but serious spinal condition requiring timely diagnosis and treatment. Surgical correction remains the gold standard, especially when neurological symptoms or tethering are present. With modern imaging, surgical expertise, and multidisciplinary care, patients with this condition can achieve excellent outcomes and improved quality of life.
Long-term success depends on early intervention, appropriate surgical management, and consistent rehabilitation. Parents and patients should work closely with a team of specialists to ensure the best course of action and long-term support.